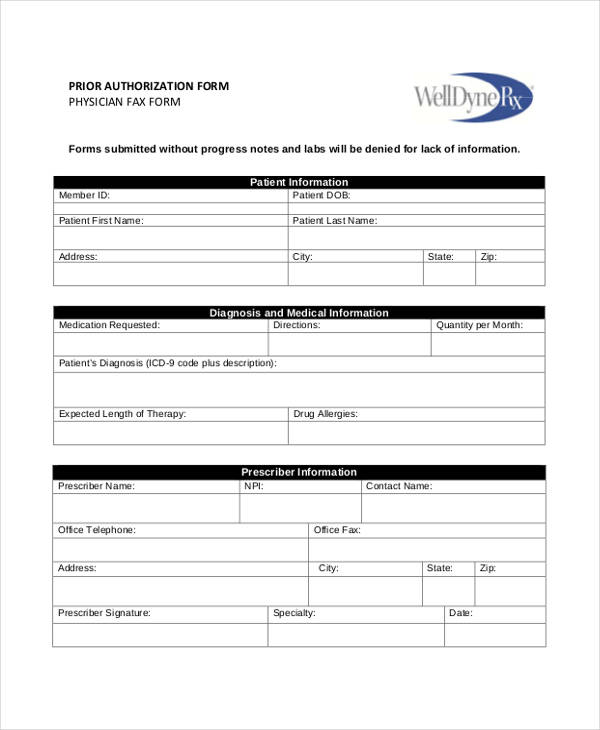
Standard Prior Authorization Form
Standard Prior Authorization Form - This form may contain multiple pages. Visit go.covermymeds.com/optumrx to begin using this free service. The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. Standard prior authorization requests are processed within 14 calendar days of receipt. Standard prior authorization requests are processed within 14 calendar days of receipt. Prior authorization information and forms for providers. Prior authorization, health care, healthcare, community health choice created date:
Allow at least 24 hours for review. Please complete all pages to avoid a delay in our decision. Standard prior authorization requests are processed within 14 calendar days of receipt. 5am to 10pm pacific / sat:
Please complete all pages to avoid a delay in our decision. Prior authorization information and forms for providers. It is important to note that an eligibility and benefits inquiry should be completed first to confirm eligibility, verify coverage, and determine To prevent delays in processing time, please provide completed documentation specific to this request. Allow at least 24 hours for review. Visit go.covermymeds.com/optumrx to begin using this free service.
MA Standard Form for Medication Prior Authorization Requests 20162021
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Fillable Standard Prior Authorization Request Form United Healthcare
Bcbs Of Mississippi Prior Authorization Form Fill Online, Printable
Fillable Form 61211 Prescription Drug Prior Authorization Request
FREE 13+ Prior Authorization Forms in PDF MS Word
Allow at least 24 hours for review. The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. Standard prior authorization requests are processed within 14 calendar days of receipt. This form intended to assist providers by streamlining the data submission process for selected services that require prior authorization. Prior authorization information and forms for providers.
It is intended to assist providers by streamlining the data submission process for selected services that require prior authorization. Texas department of insurance keywords: Member information prescriber information member name: It is important to note that an eligibility and benefits inquiry should be completed first to confirm eligibility, verify coverage, and determine
Standard Prior Authorization Requests Are Processed Within 14 Calendar Days Of Receipt.
Please complete all pages to avoid a delay in our decision. 5am to 10pm pacific / sat: Prior authorization request form please complete this entire form and fax it to: Prior authorization information and forms for providers.
It Is Important To Note That An Eligibility And Benefits Inquiry Should Be Completed First To Confirm Eligibility, Verify Coverage, And Determine
It is intended to assist providers by streamlining the data submission process for selected services that require prior authorization. Beginning september 1, 2015, health benefit plan issuers must accept the texas standard prior authorization request form for health care services if the plan requires prior authorization of a health care service. Prior authorization, health care, healthcare, community health choice created date: Member information prescriber information member name:
This Form Intended To Assist Providers By Streamlining The Data Submission Process For Selected Services That Require Prior Authorization.
Allow at least 24 hours for review. To prevent delays in processing time, please provide completed documentation specific to this request. The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. Submit a new prior auth, get prescription requirements, or submit case updates for specialties.
Texas Department Of Insurance Keywords:
Standard prior authorization requests are processed within 14 calendar days of receipt. Visit go.covermymeds.com/optumrx to begin using this free service. This form may contain multiple pages.
The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. It is intended to assist providers by streamlining the data submission process for selected services that require prior authorization. This form may contain multiple pages. It is important to note that an eligibility and benefits inquiry should be completed first to confirm eligibility, verify coverage, and determine Prior authorization, health care, healthcare, community health choice created date: